About Us
Executive Editor:Publishing house "Academy of Natural History"
Editorial Board:
Asgarov S. (Azerbaijan), Alakbarov M. (Azerbaijan), Aliev Z. (Azerbaijan), Babayev N. (Uzbekistan), Chiladze G. (Georgia), Datskovsky I. (Israel), Garbuz I. (Moldova), Gleizer S. (Germany), Ershina A. (Kazakhstan), Kobzev D. (Switzerland), Kohl O. (Germany), Ktshanyan M. (Armenia), Lande D. (Ukraine), Ledvanov M. (Russia), Makats V. (Ukraine), Miletic L. (Serbia), Moskovkin V. (Ukraine), Murzagaliyeva A. (Kazakhstan), Novikov A. (Ukraine), Rahimov R. (Uzbekistan), Romanchuk A. (Ukraine), Shamshiev B. (Kyrgyzstan), Usheva M. (Bulgaria), Vasileva M. (Bulgar).
Materials of the conference "EDUCATION AND SCIENCE WITHOUT BORDERS"
1. Introduction
The high rate of disability and mortality among patients with Diabetes Mellitus (DM) is mainly caused by cardiovascular disorders. The pathogenic effect of a number of specific factors (hyperglycemia, hyperinsulinemia, insulin resistance) accelerates the development and progression of the diseases connected with atherosclerosis. They are the main causes of death among population of industrialized countries. The incidence of cardiovascular disease is 3-4 times higher among patients with Type 2 DM in comparison with patients having normal carbohydrate metabolism. However, atypical clinical course of coronary heart disease makes diagnosis of coronary insufficiency among patients with DM rather difficult. It results in later detection of disease, i.e. the disease is often detected on the stage of severe complications such as sudden death or circulatory failure [1]. According to Thomas Killip [2], asymptomatic myocardial ischemia occurs 2-4 times more often in diabetes, while Cohn P.F. and Fox K.M. [3] say about 5-fold increased risk of cardiac mortality among patients with asymptomatic myocardial ischemia. It should be noted that the presence of silent myocardial ischemia increases the risk of complications such as acute myocardial infarction and unstable angina [4].
Although pathogenetic mechanisms of the appearance of silent and pain ischemia are considered to be the same and they are caused by mismatch between myocardial oxygen demand and coronary blood flow we still do not have a clear answer on the question about causes of asymptomatic myocardial ischemia.
The absence of pain among patients with DM is connected with loss of sensitivity of opioid receptors to adenosine which is one of the mediators of cardiac pain [3]. Other researchers believe that the main cause of the development of silent myocardial ischemia is diabetic autonomic neuropathy [5;6]. According to Kempler P. [7], 24-hour monitoring showed that 64.7% patients having DM with diabetic autonomic neuropathy suffered silent ischemia while only 4.1% patients having DM without diabetic autonomic neuropathy suffered silent ischemia.
Undoubtedly, diagnostic methods allowing the detection of disease before the development of dangerous conditions are important in the absence of characteristic clinical symptoms among patients with DM. Early diagnosis of coronary heart disease is particularly necessary.
The role of endothelial dysfunction in the formation of vascular complications attracts attention of clinicians. The vascular endothelium certainly plays a key role in maintaining normal vascular tone and structure, local homeostasis and processes of cell proliferation of the vascular wall [8, 9]. The vascular endothelium is considered to be metabolically active tissue formed by a corporation of specialized cells. It secretes both vasoconstrictors (angiotensin II, endothelin, free radicals of incompletely oxidized fatty acids, prostaglandin F2 alpha, thromboxane) and vasodilators (nitric oxide (NO), endothelial hyperpolarizing factor, prostacyclin), their effects are balanced under physiological conditions. The dysfunction of endothelial cells causes increased vascular permeability for macromolecules [10], changes in the level of vasoactive substances and vascular expansion and vasospasm respectively [11; 12] and change in the balance of coagulation and anticoagulation systems [13]. However, endothelial dysfunction most often leads to changes in the vascular lumen. Endothelial cell dysfunction is considered to be the change in the vascular response to the delivery acetylcholine into the bloodstream and hyperemia which normally lead to vasodilatation due to release of NO.
In DM the ability of endothelial cells to synthesize NO is reduced [14; 15], the ability of endothelial cells to release relaxing factors decreases while the formation of vasoconstrictive factors persists or increases, i.e. the imbalance between the neurotransmitters providing the best rate for all endothelium-dependent processes is formed. This condition is defined as endothelial dysfunction. The major manifestations of endothelial dysfunction are violation of the endothelium relaxation of blood vessels and increased adhesiveness of endothelial lining [16].
As Tooke J. noted, insulin may affect the endothelium of blood vessels in two ways causing them to either expand or spasm [17]. Binding to its receptors on the surface of endothelial cells insulin may act in two ways. The first way is an activation of NO secretion through the insulin receptor substrate 1 and substrate 2 (IRS-1, IRS-2) and phosphatidylinositol-3-kinase (PI3-K). This mechanism provides a vasodilator and antiatherogenic properties of insulin; it is involved in insulin-dependent delivery of glucose into cells. The second way is implementation of the mitogenic properties of insulin through a cascade of mediators (ras, raf, MEK) that increase the activity of mitogen-activated protein kinase, which ends with cell proliferation and migration of smooth muscle cells, activation of vasoconstrictor factor endothelin-1 and increased blood pressure [18]. The first mechanism appeared not to function in conditions of insulin resistance. It was the first way which was resistant to insulin; therefore, NO molecule was not synthesized. At the same time, the second mechanism retains its high activity, so, hyperinsulinemia has atherogenic effects.
Endothelial dysfunction of the coronary arteries manifests in reduced coronary flow reserve, inability of vessels to adequate expansion with an increase in myocardial oxygen demand. It has a significant influence on the occurrence and progression of ischemia. Changes in vascular reactivity have an impact on atherogenesis processes, hyperglycemia provokes the primary foci of atheromatous lesions of the vascular wall and creates the conditions for the formation of specific cellular component atheroma [19]. Violation of endothelial function is believed to be an important independent risk factor for coronary heart disease [20], that is why the correction of endothelial dysfunction and control of traditional risk factors for atherosclerosis should be considered as a strategic line of the effective prevention of cardiovascular complications.
According to Schachinger V. and colleages [21], patients with risk of coronary atherosclerosis traditionally suffer endothelial dysfunction of the coronary vessels, but it functions as a long-term marker of the progression of atherosclerosis and cardiovascular events when coronary heart disease is diagnosed. However, this assumption is not supported by all the researchers. A significant difference in the prevalence of silent myocardial ischemia, depending on the presence of DM is a matter of opinion too.
2. The subject and the methods of the research
Having conducted our research, we investigated the relationship between the severity of silent myocardial ischemia and functional state of arteries endothelium, we studied the significance of violations of vasomotor function with the loss of the ability to flow-dependent vasodilation as a risk factor, which increases the probability of the episodes of silent myocardial ischemia among patients with Type 2 DM.
To conduct the research we formed a group of patients with stable clinical course of coronary heart disease during the previous month. All patients including people with Type 2 DM had stable sinus rhythm. The research was conducted on condition that the patients took oral antidiabetic drugs. The elimination criteria were Grade 3 hypertension (blood pressure was above 180/110 mmHg); the presence of valvular heart disease and congestive heart failure 3-4 functional class; the presence of chronic liver and renal failure; chronic lung disease with respiratory failure; a history of cerebral stroke.
We observed 128 patients (66 male and 62 female), average age was 59.3±4.7. Each patient signed an agreement to take part in our research as a volunteer. The agreement was adopted by the local ethics committee.
We included patients with coronary heart disease and Type II DM into group 1 (n=60). Duration of diabetes was 6.4±1.5 years. The level of fasting plasma glucose was 7.7±1.5 mmol/l. Group 2 (n=68) was formed by patients having coronary heart disease without violation of carbohydrate metabolism (table 1).
The complex survey included clinical and laboratory studies, 12-lead electrocardiography, Holter ECG monitoring, stress testing (Bruce R. protocol), echocardiography, and ultrasound vascular assessment of endothelium-dependent vasodilation of the brachial artery (BA).
|
Rate |
Group 1 |
Group 2 |
|
Male/Female (n) |
26 / 34 |
40 / 28 |
|
Age (years) |
59.8 ± 4.3 |
58.7 ± 4.8 |
|
Smoking (Male/Female, n) |
24 / 5 |
32 / 4 |
|
BMI (kg/м²) |
33.1 ± 3.6 |
28.7 ± 3.1 |
|
Arterial hypertension |
|
|
|
degree (n/%) I |
35 / 58.3 |
20 / 69.7 |
|
Stable angina (n): |
|
|
|
I Functional Class |
14 |
15 |
|
Burdened hereditary history |
|
|
|
DM (n/%) |
48 / 80 |
8 / 11.8 |
|
Duration of illness (years) |
|
|
|
coronary heart disease |
6.4 ± 1.5 |
5.9 ± 3.2 |
|
hyper Dyslipidemia (n/%) |
54 / 90 |
53 / 77.9 |
|
signs of CHF,% |
42 / 60 |
37 / 54.4 |
Table 1.
Clinical characteristics of patients
Note: BMI - Body Mass Index; CHF - Chronic Heart Failure; CD - Cardiovascular Disease; hyper Dyslipidemia- total cholesterol is more than 5.0 mmol/l and/or low-density lipoprotein cholesterol is more than 3 mmol/l when high density lipoprotein cholesterol is less than 1 mmol/l; n - the absolute number of individuals with this figure; % - number of persons with this figure from the total number of persons enrolled in the study.
Vascular Doppler ultrasound was conducted before 10 a.m. when a patient was fasting. The patient had a 10-minute rest before the test. During the test the patient was lying on his/her back. Having scanned the common carotid artery, the brachial artery, common femoral artery and tibial arteries we used a linear detector with the ability to visualize the image in the frequency range 5-12 Hz.
In B-mode we studied the following parameters: vascular permeability; vascular geometry (the correspondence of vascular duct to the anatomical vessel trajectory); the diameter of the vessel (intraluminal); the condition of the vascular wall (the integrity, the thickness of the intima-media (Figure 1.), echogenicity, the degree of differentiation of the layers, the shape of the surface); the state of the vessel lumen (presence, location, length, echogenicity of intraluminal structures, the degree of obstruction); the state of the perivascular tissue (presence, shape, extent, cause extravasal impact). In spectral Doppler mode, we analyzed quantitative indicators of blood flow: peak systolic blood flow velocity (Vps, cm/s); the maximum end diastolic blood flow velocity (Ved, cm/s); diastolic blood flow velocity (Vd, cm/s), evaluated in arteries with high peripheral resistance; maximum blood flow velocity, averaged over time (TAMX, cm/s); peripheral resistance index - RI.
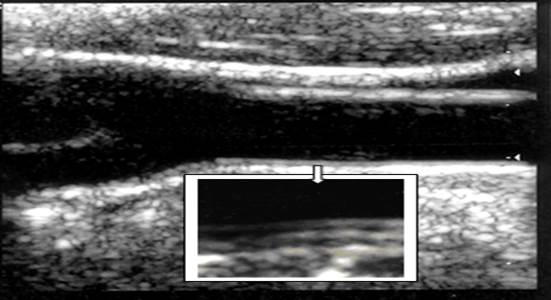
Figure 1.
Assessment of intima-media for ultrasound scanning in B-mode
To assess vasomotor function of vascular endothelium, we used a test with reactive hyperemia, i.e. detection of endothelium-dependent vasodilation of the BA by the method of Celermaer D.S. and Sorensen K.E. [22]. The sensor was located in the longitudinal section of a 3 - 4 cm above the elbow. First, the diameter of the BA and the velocity of blood flow through it were measured. Reactive hyperemia was produced by applying a sphygmomanometer cuff on the upper third of the shoulder. During 3-4 minutes we maintained the cuff pressure in this patient greater than systolic pressure by 40 mm Hg. After decompression, the next measurements were carried out in 60 seconds. Endothelium dependent vasodilatation was calculated by the following formula:
Endothelium dependent vasodilatation= ((BA diameter after the test - initial diameter of the BA)/initial diameter of the BA)×100%.
The degree of increase in BA diameter of more than 10% was regarded as a preserved endothelium dependent vasodilatation. In violation of endothelium vasomotor function of BA diameter increase was less than 10%. We got more information on the status of endothelial vasomotor function using the method of transcranial duplex scanning with the stress test, which activates the metabolic mechanisms of influence on the endothelium, i.e. breath holding test. We analyzed the nature of response to the functional stress test, taking into account the index of reactivity:
1. positive - the index of reactivity was from 1.1 to 1.4;
2. negative - the index of reactivity was 0.9 to 1.1;
3. paradoxical - the index of reactivity was less than 0.9 [23].
ECG monitoring was conducted in the ordinary daily routine of a patient. The patient was to keep a diary during ECG recording; he or she recorded the nature of his/her activities and his/her state of health in detail. Besides a computer decoding, the analysis of the results of our research included visual viewing of individual fragments of the ECG recording, which increased the reliability of conclusions. We analyzed ischemic changes, taking into account corrections of the original position in ST segment whether it was ST segment elevation or depression (Figure 2.).
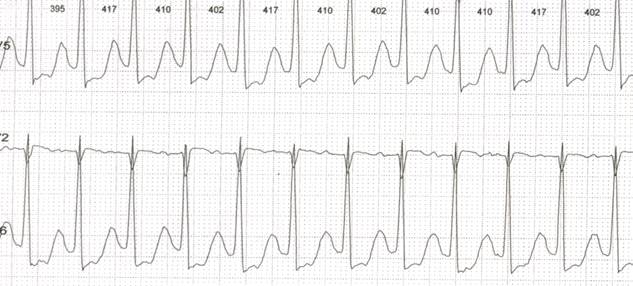
Figure 2.
Variant of ischemic ST segment depression
When evaluating each episode, we noted the presence or absence of pain (according to a patient’s diary or a marker on the monitor records; we calculated the total duration of daily depression of ST segment (daily myocardial ischemia), a maximum depth of ST segment depression (↓STmax), heart rate (HR) at the beginning of painful and painless episodes of ST displacement.
Statistical processing and analysis of the results obtained are presented in the system of statistical analysis STATISTIKA (the package of applied programs STATISTIKA by company StatSoft Inc., Version 6.0.).
3. The results of the research and the discussion
In countries that have achieved significant success in treatment and prevention of coronary heart disease, patients with DM are the only group in which the death rate from this disease has slightly decreased among men and increases among women [24]. In this connection, the data of clinical analysis and comparative evaluation of ischemic episodes based on the results of daily monitoring of ECG and stress testing in groups I and II (Table 2) are of considerable interest.
|
Rate |
Group 1 |
Group 2 |
|
The presence of SMI (n) |
56 / 93.3%* |
40 / 58.8% |
|
Number of painful episode of myocardial ischemia |
2.1 ± 0.3 |
2.1 ± 0.43 |
|
Number of silent myocardial ischemia |
2.8 ± 0.4* |
1.1 ± 0.3 |
|
DMI (min) |
45.3 ± 3.2* |
33.6 ± 2.4 |
|
PEMI (min) |
14.7 ± 2.5 |
15.2 ± 1.7 |
|
Silent myocardial ischemia (min) |
31.1 ± 2.1* |
18.6 ± 2.2 |
|
The depth of ST segment depression (mm) |
|
|
|
average |
1.53 ± 0.4 |
1.5 ± 0.2 |
|
Average heart rate(beats / min) |
|
|
|
at the beginning of PEMI |
116 ± 2.3 |
122 ± 1.8 |
|
VA during episodes of ischemia (n/%) |
12 / 20* |
8 / 11.8 |
|
The volume of work done (Watt) |
400 ± 20* |
580 ± 20 |
|
The threshold power of load (Watt) |
66.5 ± 2.3* |
83.3 ± 2.8 |
|
Time of occurrence |
|
|
|
ST segment depression (min) |
6.7 ± 0.3* |
8.6 ± 0.4 |
|
Time of pain occurrence (min) |
7.3 ± 0.4 |
8.5 ± 0.7 |
|
The number of leads with ST depression |
6.3 ± 0.4* |
4.4 ± 0.2 |
Table 2.
Comparative analysis of functional methods
Note: DMI - Daily Myocardial Ischemia (duration of ischemic episodes per day); SMI - Silent Myocardial Ischemia; PEMI - Painful Episode of Myocardial Ischemia; VA - Ventricular Arrhythmia; *- р < 0.05 – a significant difference.
In group 1 we observed periods of silent ischemia among 93.3% patients, painful episodes of myocardial ischemia were detected in the form of compressive retrosternal pain, discomfort in the chest and dyspnea among 66.7% patients. When analyzing daily trend of ST segment and patients’ diary records, we registered a combination of painful episodes of myocardial ischemia and silent myocardial ischemia in 60% cases. Only 6.7% patients with Type II DM had painful episodes of myocardial ischemia while 33.3% patients had ischemic depression episodes of ST segment without any subjective manifestations. That was a significant difference in comparison with the corresponding figures in group 2, χ2=5.4 (p<0.05).
In group 2 episodes of silent myocardial ischemia were detected in 9 (13.2%) cases during a day, the detection rate of painful episodes of myocardial ischemia was 59 (88.6%) cases, 28 (41.2%) patients having had only painful episodes of myocardial ischemia. According to diary records, 51.7% patients with coronary heart disease had a combination of painful episodes of myocardial ischemia and silent myocardial ischemia. A significant difference was obtained by assessing the duration of all episodes of myocardial ischemia during the day in group 1 and group 2, it was 45.3±3.2 min and 33.6±2.4 min< p<0.03 accordingly.
The average depth of ST segment depression did not differ significantly among patients of both groups. However, maximum depth of ST depression in group 1 exceeded the same indicator in group 2, it was 2.4±0.2 mm and 1.6±0.3 mm, p<0.05 accordingly. The value of heart rate at the beginning of pain and painless episodes did not differ significantly according to groups.
The amount of work done and threshold power were lower among patients of group 1 than patients of group 2. 85% patients of group 1 had ischemic displacement of ST segment, it was detected in more than 6-lead ECG during stress testing.
Measuring the ability to perceive pain which is associated with transient myocardial ischemia has a prognostic value in stable angina. Angina/the equivalent of angina is a signal for patients to regulate their daily physical activity.
We should note that later attack of pain with a delay relatively to the ischemic ST segment shift was detected among 27(45%) patients of group 1 during stress test. In 31 (51.7%) cases the emergence of pain coincided with the appearance of ischemic symptoms on the electrocardiogram. However, in 2 cases the pain occurred before the appearance of ST depression. Having analyzed the results, we obtained different data in group 2: the number of patients with premature/simultaneous appearance of angina/its equivalent was 85.3% and it exceeded the number of patients with late appearance of pain attack (14.7%), p<0.02. We assume that data on the detection rate during stress testing of patients with the later occurrence of the attack/equivalent of angina with respect to ischemic ST segment shift (45% and 14.7% - p<0.03 respectively), obtained in group 1 in comparison with group 2 may be explained by increased sensitivity to pain among patients with insulin resistant diabetes. It is associated with a change in neuronal component of pain inhibition system, which includes not only the conductors of pain sensitivity, but peripheral receptors in the myocardium.
The data obtained are consistent with the results of daily monitoring of the ECG. The probability of occurrence of asymptomatic episodes of ST depression is significantly higher among patients having coronary heart disease and DM than among patients with coronary heart disease without violation of carbohydrate metabolism. Ratio silent myocardial ischemia/painful episodes of myocardial ischemia was 1.29 in group 1, and it exceeded the same indicator among patients of group 2 – 0.52 (χ2=3.84, р<0.05).
However, in our opinion, the pathogenesis of silent myocardial ischemia with violation of carbohydrate metabolism is complex; it appears to be related not only to autonomous cardiac neuropathy, but also to the development of angiopathy, microcirculation disturbance.
It should be noted that the presence and severity of endothelial dysfunction among patients with documented lesions of coronary arteries is a proven marker of poor prognosis [25]. However, this large-scale destruction of the vascular bed does not occur for any other disease, like DM; this is due to the influence of hyperglycemia on the primary target cell, vascular endothelium. Studies carried out in a clinical setting, showed that in DM endothelial dysfunction is associated with microangiopathy and atherosclerosis [26; 27].
When studying functional characteristics of vascular endothelium in the analyzed groups we paid special attention to the results on detecting endothelium-dependent vasodilation of the BA (Table 3).
|
Rate |
Group 1 |
Group 2 |
||
|
initially |
after the test |
initially |
after the test |
|
|
Diameter of the BA (mm) |
3.8 ± 0.19 |
3.94 ± 0.11** |
4.07 ± 0.18 |
4.57 ± 0.12* |
|
Vps (m/s) |
0.62 ± 0.04 |
0.84 ± 0.06 |
0.64 ± 0.05 |
0.92 ± 0.04* |
|
Ved (m/s) |
0.10 ± 0.05 |
0.13 ± 0.03 |
0.12 ± 0.06 |
0.16 ± 0.03* |
|
ТАМX (m/s) |
0.12 ± 0.03 |
0.29 ± 0.06** |
0.13± 0.02 |
0.43 ± 0.04* |
|
EDV BA (%) |
3.7 ± 1.1** |
12.3 ± 2.1% |
||
Table 3.
Performance test with reactive hyperemia in groups of patients
Note: Vps - Peak systolic blood flow velocity; Ved - maximum end diastolic flow velocity; ТАМX - the time-averaged maximum velocity of blood flow; EDV BA - endothelium dependent vasodilation of brachial artery; *- р< 0.05 - reliability of differences between parameters obtained initially and after the test; ** - р< 0.05 - difference is reliable between indicators of group 1 and group 2.
The original diameter of the BA did not differ significantly in the analyzed groups; it was 3.8±0.19 mm and 4.07±0.18 mm, respectively. Evaluating the mechanism of endothelial regulation of vascular tone among patients in group 1, in the presence of DM, we diagnosed vasomotor endothelial dysfunction induced by shear stress in all cases. The diameter of the BA increased after removal of the cuff by only 3.7±1.1% of the initial indicator in the group. At the same time 53.3% (32) of patients had violation of endothelial vasomotor function as a lack of vasodilating effect, i.e., less than 10% of the original value, 26.7% (16) of patients had violation of endothelial vasomotor function as the lack of increase in BA diameter, and 20% (12) of patients had violation of endothelial vasomotor function in the form of pathological vasoconstriction.
An interesting fact is that endothelial dysfunction induced by shear stress was detected in the form of lack of increase in BA diameter and pathological vasoconstriction among patients with Type II DM (33.3% of the total number of patients in group 1) having episodes of silent myocardial ischemia without subjective symptoms, it was 15% и 18.3% of cases accordingly.
Correlation analysis showed a significant negative correlation between endothelial dysfunction and the presence of silent myocardial ischemia (R= -0.68, p<0.01), duration of episodes of silent myocardial ischemia (R= -0.53, p<0.01), lag time of pain in relation to coronary ST depression (R= -0.61, p<0.01) in group 1.
We have received reliable dependence of endothelium dependent vasodilation from the functional class (FC) of angina (R= -0.4215, p <0.04): endothelium dependent vasodilation was 2.4±0.3% in stable angina of FC III, that was significantly less than similar indicator among patients with angina of FC I and FC II, it was 5.2± 0.2% and 4.05±0.15% (p <0.03), respectively.
In group 2 index of endothelium dependent vasodilation of BA was 12.3±2.1%. We did not reveal any violations of the vasomotor function of vascular endothelium among 44.1% (30) of patients of this group (endothelium dependent vasodilation was more than 10%). Endothelial dysfunction was registered in 38 (40%) cases: in 29 (42.6%) cases patients suffered lack of growth in BA diameter (endothelium dependent vasodilation was less than 10%), 7 (10.3%) patients had no increase in BA diameter and only 2(3%) patients suffered pathological vasoconstriction.
In Doppler test of linear velocity rates of blood flow of BA (peak systolic blood flow velocity (Vps), maximum end diastolic flow velocity (Ved)), the time-averaged maximum velocity of blood flow (ТАМX) did not differ significantly in the groups. However, the degree of increase of the velocity indicators in comparison with reactive hyperemia test was significantly higher in group 2, which also shows a decrease in vasodilating reserve in group 2.
Table 4 presents the results of the analysis of quantitative and qualitative assessment of intima-media complex (IMC) of the arteries of the lower limb arteries, common carotid artery (CCA) and the analysis of cerebrovascular reactivity in these tests with breath-holding.
The thickness of IMC of patients in group 1 was 1.24±0,06 mm in the CCA, in the common femoral artery (CFA) it was 1.32±0.07 mm, the numerical values of these indices were higher than similar indicators among patients of group 2, p<0.05. Doing a qualitative analysis of the IMC state we revealed three different types of changes among patients with Type II DM: diffuse uniform thickening of the IMC with the appearance of additional layers of high and low echogenicity in the structure of the intima-media in the CFA, the superficial femoral artery (SFA), the popliteal artery (PA), the posterior tibial artery (PTA), the anterior tibial artery (ATA) (100% patients); in the CCA (95% patients); presence of multiple local zones of increased echogenicity with visualization of atherosclerotic plaques in the structure of IMC (95% were in the PTA and the ATA, 80% were in the PA, 71.7% were in the CFA and SFA; 66.7% patients had it the CCA), increased echogenicity of IMC with the complete loss of its differentiation into the layers (13% of cases were in the CCA).
|
Rate |
Group 1 |
Group 2 |
|
Thickness of IMC of the CFA (mm) |
1.32 ± 0.07 |
1.18 ± 0.09 |
|
The presence of atherosclerotic plaques in the arteries of the lower limbs (n/%) |
57 / 95 |
39 / 57.4* |
|
Thickness of IMC of CCA (mm) |
1.24 ± 0,06 |
1.12 ± 0.08 |
|
The presence of atherosclerotic plaques in CCA (n/%) |
40 / 66.7 |
29 / 42.6 |
|
initial indices of blood flow in the MCA |
||
|
Vps (cm/s) |
75.3 ± 11.4** |
79.2 ± 9.2 |
|
TAMX (cm/s) |
37. 7 ± 8.5** |
39.6 ± 7.63 |
|
RI |
0.52 ± 0.06** |
0.6 ± 0.05 |
|
indices of blood flow in the MCA after the test with breath-holding |
||
|
Vps (cm/s) |
76.2 ± 12.2** |
96.2 ± 10.61* |
|
TAMX (cm/s) |
38.2 ± 4.9** |
57.02 ± 11.2* |
|
RI |
0.51 ±0.10** |
0.55 ± 0.09* |
Table 4.
Analysis of the intima-media complex of the arteries in the two groups with the assessment of cerebrovascular reactivity
Note: CFA - common femoral artery; CCA - common carotid artery; MCA - middle cerebral artery; Vps - Peak systolic blood flow velocity; ТАМX - the time-averaged maximum velocity of blood flow; RI - index of peripheral resistance; *- р< 0.05 - reliability of differences between parameters obtained initially and after the test; ** - р< 0.05 - difference is reliable between indicators of group 1 and group 2
Atherosclerotic vascular changes suffered by patients without DM differed from those of patients with DM. In group 2 we recorded diffuse irregular thickening of the intima-media complex with an increase of its echogenicity, sometimes with loss of differentiation of the layers mainly in large arteries (55.9% cases were in the CCA, 70.6% were in the CFA and SFA, 54.4% were in the PA, 45.6% were in the PTA and ATA), combined with abnormal thickening and the presence of atherosclerotic plaques (42.6% cases were in the CCA, 57.4% were in the CFA and SFA).
The analysis of cerebral reactivity in group 1 showed that the response on the metabolic stimulation was negative among 52 (86.7%) patients; 6 (10%) patients had a paradoxical reaction with reduced velocity parameters of the MCA.
Initial indices in group 2 did not differ significantly from the corresponding figures in group 1. However, having done breath holding test, we had a reliable increase by 16% in Vps and by 30% in TAMX (p<0.05). The reaction on the metabolic vasodilating test in the MCA was negative only in 5 (7.35%) cases.
These data suggest that patients with coronary heart disease and violation of carbohydrate metabolism in the peripheral blood vessels suffered the changes which had two-side and diffuse nature with many sections of lesions, whereas patients without diabetes usually had changes occurring on one side of the peripheral arteries and/or lesion of a single segment of arterial tree. We calculated a negative correlation of thickness of IMC and endothelium dependent vasodilatation (R= -0.8743, р<0.01).
Neurohumoral disorders should be taken into account in the process of remodeling of the heart and blood vessels. Renin-angiotensin-aldosterone system (RAAS) is very important in the pathophysiological processes that eventually lead to cardiovascular remodeling, increasing the risk of cardiovascular complications [28]. Drug effect on the RAAS should be considered the standard therapeutic procedure. In this connection, study and discussion of metabolic, vascular and organ-protective effects of drugs, suppressing the activity of the RAAS are of special importance. To exclude the development of left ventricular remodeling, impaired left ventricular diastolic function and vasomotor endothelial dysfunction of the arteries from the life of patients with Type II DM is not possible. However, when treating the patients, specific efforts should be directed to slow the progression of these disorders.
We evaluated the effect of antagonist of telmisartan angiotensin II receptor on blood pressure (BP), carbohydrate and lipid metabolism, the parameters of intracardiac hemodynamics and left ventricular remodeling, endothelial vasomotor function of arteries. For 40 weeks Telmisartan - Mikardis (Boehringer Ingelheim Pharma) was prescribed to 60 patients with coronary heart disease and Type II DM in addition to standard therapy (antiplatelet, statins, peripheral vasodilators, and calcium antagonist in the pro re nata mode, oral hypoglycemic agents). The average dose for the group was 80 mg per day during the first weeks, 40 mg/day were prescribed to 24 patients during the next weeks and 36 patients took 80 mg/day).
The choice of telmisartan which is from the group of angiotensin receptor antagonists (ARA) is dictated by the results of investigations, according to which there may be a substantial difference in the influence of drugs on metabolic processes within the ARA drug group [29; 30]. This difference is explained by different ability of individual ARA to activate proliferator activation receptors by peroxisome of γ type (PPAR-γ), i.e. nuclear factors discovered by their ability to respond to xenobiotics by peroxisomal proliferation in the liver. According to Bakris G. [29], attention to PPAR is paid due to their key role in the regulation of lipid and carbohydrate metabolism in general and in the formation of insulin resistance and Type II DM in particular. The synthesis of PPAR-γ activators gives additional possibilities in the treatment of Type II DM and metabolic syndrome. However, the breadth of the spectrum of their effects allows us to think about the potential of their use in primary and secondary prevention of cardiovascular complications.
To assess the degree of compensation of carbohydrate metabolism, we measured the following indicators: levels of fasting and postprandial (2 hours after eating) blood glucose (mmol/l) at each visit, glycated hemoglobin (HbA1c, %), initially and after 40 weeks of observation.
85% of patients with Type II DM and stable angina who took telmisartan in addition to standard therapy showed subjective improvement in physical condition. Having done the analysis of anginal attacks in the group, we noted a significant reduction (from 21.7 ± 2.1 to 14.3 ± 1.1 episodes) in angina attacks per week and a reduced need (from 12.8 ± 1.3 to 5.3 ± 1.1 tablets) for short-nitroglycerin per week by the 40th week of observation.
According to clinical measurements of blood pressure (BP) a significant reduction in office systolic (SBP) blood pressure and diastolic blood pressure (DBP) was observed among patients being treated with telmisartan during the test appearances, 95% of patients having target BP level of SBP. Target BP level of DBP was in 96.7% cases, p <0.05.
According to the ambulatory blood pressure monitoring (ABPM), abnormal profile of blood pressure trend was observed among 88.3% of patients, most of them (75%) forming the category of "non-dippers" (patients with lack of normal physiological reduction in blood pressure at night). However, we identified cases of distorted circadian rhythm with a predominantly nocturnal hypertension (13.3%), i.e. the group of "night-pickers".
After 40 weeks of the therapy we received reduction in daily average SBP and DBP, time index of hypertension for 24 hours, the variability in SBP and DBP (p<0.05) (Table 5).
We observed a normalization of circadian BP profile among 85% of patients that was 96.2% of patients with abnormal circadian rhythm (non-dipper and night-picker). Therapy with telmisartan allowed us to reduce indicators of the magnitude and rate of morning increase in BP. Thus, the magnitude of morning increase in SBP decreased by 49% and the magnitude of morning increase in DBP decreased by 51.4% while the rate of morning increase in SBP decreased by 69% and the rate of morning increase in DBP decreased by 62.9% (p<0,03).
|
Rate |
Initial |
After 40 weeks |
|
circadian blood pressure monitoring indicators |
||
|
Daily average SBP (mmHg) |
148.4 ± 11.3* |
127.1 ± 3.3 |
|
Daily average DBP (mmHg) |
89.3 ± 6.7* |
77.2 ± 3.1 |
|
The daily variability of SBP (mmHg) |
21.9 ± 2.8* |
15.2 ± 1.7 |
|
The daily variability of DBP (mmHg) |
16.4 ± 2.3* |
9.9 ± 1.1 |
|
Time index of systolic hypertension in 24 hours (%) |
80.4 ± 5.3* |
32.3 ± 5.2 |
|
Time index of diastolic hypertension in 24 hours (%) |
66.7 ± 3.4* |
22.3 ± 2.5 |
|
The rate morning increase of SBP (mmHg/h) |
29.7 ± 3.2 |
9.2 ± 1.4 |
|
The rate morning increase of DBP (mmHg/h) |
17.8 ± 3.1 |
6.6 ± 1.0 |
|
circadian ECG monitoring indicators |
||
|
DMI (min) |
45.3 ± 3.2* |
20.7±1.4 |
|
PEMI (min) |
14.7 ± 2.5 |
11.3 ± 1.3 |
|
SMI (min) |
31.1 ± 2.1* |
9.5 ± 1.5 |
Table 5.
Dynamics of functional parameters during therapy with telmisartan
Note: differences were significant between the numerical values of initial rates and rates after 40 weeks of therapy with telmisartan.
We indicated the positive dynamics of indicators characterizing the process of left ventricular remodeling: a decrease in end-diastolic volume (EDV) and end-systolic volume (ESV) by 7.5% and 8.4%, respectively, and an increase in ejection fraction by 6.6%, p<0.05. The fraction of systolic shortening of the anterior-posterior size of the left ventricular increased by 8.2%.
Daily rates of myocardial ischemia have undergone significant changes: number of ischemic episodes decreased from 4.8±0.34 to 2.3±0.3; maximum depth of ST segment depression decreased from 2.5 ± 0.2 mm to 1.7 ± 0.1 mm; duration of ischemic episodes decreased from 45.3±3.2 min to 20.7 ± 1.4 min. We should emphasize that the positive dynamics was indicated in most cases when we analyzed data on silent myocardial ischemia: duration of all episodes of silent myocardial ischemia decreased during the day (p<0.05) and the number of episodes of silent myocardial ischemia decreased from 2.8±0.4 to 1.2±0.2 per day too.
We explain the result obtained not only by improved circadian BP profile and adequate control, but also by the presumable ability of the drug to effect myocardial blood flow making coronary vasodilation and redistributing blood flow towards the subendocardial layers of myocardium, which are particularly vulnerable to ischemia. We established the correlation of the duration of painless ST segment depression and a daily index of SBP (R= -0.53, p<0.02), daily index of DBP (R= -0.61, p<0.03).
These reactive hyperemia tests allowed us to indicate the improvement of vasomotor function induced by shear stress, endothelium dependent vasodilatation increasing from 3.7±1.1% to 7.2±1.1%. We had positive dynamics of velocity indicators: peak systolic blood flow velocity increased from 0.84±0.06 m/s to 0.94±0.04 m/s (р<0.05); maximum diastolic blood flow velocity increased from 0.13±0.03 m/s to 0.18±0.03 m/s (р<0.05); time-averaged maximum flow velocity increased from 0.29±0.06 to 0.46±0.04 (р<0.05).
Individual analysis of the endothelium dependent vasodilatation dynamics during treatment with telmisartan showed that the number of patients with impaired endothelial function decreased to 51.7%, while the number of persons with pathological vasoconstriction/vasodilation in the absence of performing the test with reactive hyperemia decreased by 23.3% (Figure 3.).
Recovery of adequate dilatation response of vessels to reactive hyperemia test is a necessary link in the chain of effective therapeutic intervention aimed at reducing of cardiovascular risk. It is known that activation of the RAAS is an indispensable part of the pathogenesis of endothelial dysfunction, so the use of these drugs in its correction seems most reasonable at present. The mechanism of endothelial function improvement by drugs blocking the RAAS is explained at present by the elimination of the adverse effects of ATII [31; 32] having a powerful vasoconstriction influence by stimulating of AT1-receptor of vascular smooth muscle cells. It is also considered as an inducer of oxidative stress with production of superoxide anion by simulation of nicotinamide-adenine-dinucleotide-phosphate; the action of angiotensin II is opposite to the action of nitric oxide, i.e. oxidase.
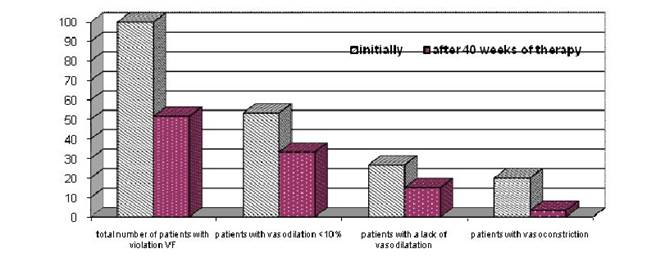
Note: The data are presented in percents, VF - vasomotor function.
Figure 3.
Correction of endothelial vasomotor dysfunction of arteries during the course therapy with telmisartan.
We also associate the resulting effect of telmisartan to improve vasomotor endothelial function with the complicated mechanism of regulation of the circadian blood pressure variability. In this sense, control of blood pressure with ARA group drugs can be considered reasonable in terms of impact on the pathophysiological mechanisms leading to the morning increase of BP, and in terms of protection of patients at the beginning of drug action during the regular morning drug intake. This fact may be proved by revealed correlation dependence of the endothelium dependent vasodilatation dynamics from the time index of hypertension on DBP for 24 hours (R= -0.64, p<0.003) and the daily index (R= 0.54, p<0.02).
Conducting therapy with telmisartan, we noted a significant decrease in glycated hemoglobin level from 8.41±0.2% to 6.5±0.4%, a decrease of fasting plasma glucose from 8.72±0.35 mmol/l to 6.67±0.4 mmol/l (p<0.02) and a decrease of postprandial blood glucose level from 9.2±1.68 to 8.5±1.38 mmol/l (p<0.05). The number of patients who achieved compensation of carbohydrate metabolism in three indices of "glycemic triad" rose from 10% to 23.3%. We indicated the correlation dependence of endothelium dependent vasodilation dynamics from glycated hemoglobin (R= -0.56, p <0.05).
We evaluated the dynamics of lipid metabolism indices among patients with Type II DM during therapy with telmisartan. After 40 weeks we noted an improvement of laboratory parameters which showed a decrease in total cholesterol by 23%, low-density lipoprotein cholesterol by 21%, triglycerides by 26% (p<0.05). We explain it by the increase in sensitivity of tissues to insulin and decreased hyperinsulinemia, which largely determine the metabolism of lipids in the body.
The data obtained allow us to state that telmisartan has a positive metabolic effect, which has an additional metabolic effect along with mechanisms of local pancreatic RAAS blocking being common for all the ARA drugs [33], i.e. agonistic effect on PPAR-ɣ-receptors, which control the activity of cytokines - the regulators of intercellular interactions, leading to a positive influence on carbohydrate and lipid metabolism and reduction of severity of insulin resistance (IR) phenomenon.
4. The conclusion
So, patients with coronary heart disease and Type II DM had silent myocardial ischemia 2 times more often than patients with coronary heart disease who had no disorders of carbohydrate metabolism. Patients with coronary heart disease and Type II DM had dominating daily duration of episodes of myocardial ischemia and a maximum depth of ST segment depression. Besides, they had reduced endothelium-dependent vasodilation reaction (endothelium-dependent vasodilation =3.7±1.1%). Violation of the functional state of the vascular endothelium correlates with the registration frequency (R= -0.68, p<0.05) and duration of episodes of silent myocardial ischemia (R= -0.53, p<0.01). Endothelial dysfunction of the coronary arteries which is manifested by blood vessels inability to adequate increase in conditions of increased myocardial oxygen demand has an influence on the genesis and progression of ischemia.
The results obtained during our research prove that metabolic factors play a significant role in the development of endothelial dysfunction. To predict vascular complications it is necessary to assess vasomotor function of arteries endothelium among patients with Type II DM.
Prescribing receptor antagonists of angiotensin II, we take into account organ-protective effects of drugs, manifested by the selective blockade of the tissue RAAS and indirect stimulation of the AT2-receptors during their long-term intake.
It is considered to be a proved fact [34; 35] that the increased activity of tissue RAAS causes long-term effects of angiotensin II (AII), which are manifested in structural and functional changes in target organs and lead to the development of a number of pathological processes such as hypertrophy, miofibroz, atherosclerotic lesion of vessels. The research [36] showed that a human body had alternative ways with chymase, cathepsin G, serine proteases in addition to ACE-dependent pathway of conversion of angiotensin I to angiotensin II. According to Elmfeldt D. and colleagues [37], chymase dependent formation of AII prevails in myocardial interstitium and adventitia and media of vessels, whereas ACE-dependent formation prevails in blood plasma. This fact explains the risk of AII escape phenomenon during the long-term intake of ACE (angiotensin-converting enzyme).
Additional metabolic effect of selective antagonist of AT1-receptor of telmisartan is agonistic effect on PPAR-ɣ-receptors, which is manifested in a significantly improved glucose and lipid profiles indices. This effect allows us to consider it as the drug of choice in the treatment of patients suffering a combination of metabolic disorders, hypertension in clinical manifestations of stable angina. Correlation analysis showed the dependence of HbA1c on the daily duration of ST depression episodes (R=0.66, p<0.01) and the duration of asymptomatic ST depression (R=0.75, p<0.02).
Modern methods in treatment of patients with coronary heart disease and DM allow using a scheme of the multi-component therapy, in which much attention is given to the improvement of endothelial function. It leads to the concurrent positive therapeutic effects of telmisartan on major links in the chain of cardiovascular complications in Type II DM improving glucose and blood lipid profile indices, a more pronounced organ protective effect. In addition, it directly prevents the development of ischemia and its main clinical manifestation.
Summary
The development of ischemic episodes in the absence of pain or angina equivalents (e.g., dyspnea, arrhythmias) is possible when a patient has coronary heart disease. Atypical clinical course makes diagnosis of coronary insufficiency with disorders of carbohydrate metabolism rather difficult. Having done the analysis of the daily trend of ST segment and the diary records of patients with DM we have identified a silent myocardial ischemia in 93.3% cases, 60% patients having a combination of painful and painless episodes of myocardial ischemia. 33.3% from 93.3% cases of ischemic episodes of ST segment depression were not accompanied by any subjective symptoms. Patients with coronary heart disease and DM have reduced endothelium-dependent vasodilation reaction (endothelium-dependent vasodilation =3.7±1.1%). Violation of the functional state of the vascular endothelium correlates with the registration frequency (R= -0.68, p<0.05) and duration of episodes of silent myocardial ischemia (R= -0.53, p<0.01).
Abbreviations
ABPM - ambulatory blood pressure monitoring
ARA - angiotensin receptor antagonists
ATII - angiotensin II
BP - blood pressure
CHD - Coronary Heart Disease
CHF - chronic heart failure
DM - Diabetes Mellitus
DB2 - Type 2 Diabetes Mellitus
ECG – electrocardiogram
ED - endothelial dysfunction
FC - Functional Class
IMC - Intima-Media Complex
IR - insulin resistance
NO - Nitrogen Oxide
PEMI - Painful Episode of Myocardial Ischemia
PPAR - peroxisome proliferator activating ɣ-receptor
RAAS - Renin-angiotensin-aldosterone system
2. T Killip, Silent Myocardial Ischemia: Some good news. Circulation 1997 95 1992 93
3. P. F Cohn, K. M Fox, Silent myocardial ischemia. Circulation 2003 108 1263 90
4. A. W Schoenenberger, P Jamshidi, R Kobza, et al Progression of coronary artery disease during long-term follow-up of the Swiss Interventional Study on Silent Ischemia Type II (SWISSI II). Clin. Cardiol 2010 33 5 289 95
5. G Jermendy, Z Davidovits, Khoor S: Silent coronary artery disease in diabetic patients with cardiac autonomic neuropathy. Diabetes Care 1994 17 1231 32
6. A Gokcel, M Aydin, F Yalcin, Silent coronary artery disease in patients with type 2 diabetes mellitus. Acta Diabetol 2003 40 176 80
7. P Kempler, Neuropathies. Pathomechanism, clinical presentation, diagnosis, therapy/ Ed. by P. Kempler. Springer; 2002
8. V Dzau, K Bernstein, D Celermajer, et al Pathophysiologic and therapeutic implications of tissue ACE: a consensus report. Cardiovasc Drugs Ther 2002 16 2 149 60
9. D. S Celermajer, Endothelial dysfunction: does it matter? Is it relevant? J Amer Coll Cardiology 1997 30 325 33
10. D. A Antonetti, A. J Barber, E Lieth, et al Vascular permeability in experimental diabetes is associated with reduced endothelial occludin content: occludin expression is decreased in experimental diabetic retinopathy. Diabetes 1998 47 1953 59
11. E Bassenge, J Zanziger, Nitrates in different vascular beds, nitrate tolerance, and interactions with endothelial function. Am. J. Cardiol 1992 28 371 74
12. P Cacoub, R Dorent, P Nataf, et al Endothelin-1 in the lungs of patients with pulmonary hypertension. Cardiovasc Res 1997 33 1 196 200
13. K Kario, T Matsuo, H Kobayashi, et al Hyperinsulinemia and hemostatic abnormalities are associated with silent lacunar cerebral infarcts in elderly hypertensive subjects. J Am Coll Cardiol 2001 37 871 77
14. T Luscher, R. R Wenzel, G Noll, Local regulation of the coronary circulation in health and disease: role of nitric oxide and endothelin. Europ Heart J 1995Suppl. C): 51 58
15. M Cipolla, Diabetes and Endothelial Dysfunction: A Clinical Perspective. Endocr Rev 2001 22 1 36 52
16. P. M Vanhoutte, C. M Boulanger, Endotheliumdependent responses in hypertension. Hypertens Res 1995 18 2 87 98
17. J. E Tooke, The association between insulin resistance and endotheliopathy. Diab Obes Metab 1999 1 23 31
18. F Folli, M. J Saad, L Velloso, et al Crosstalk between insulin and angiotensin II signaling systems. Exp Clin Endocrinol Diabetes 1999 107 133 39
19. A Ceriello, A Cavarape, L Martinelli, et al The post-prandial state in type 2 diabetes and endothelial dysfunction: effects of insulin aspart. Diabet Med 2004 21 171 75
20. A. L Hinderliter, M Caugher, Assessing endothelial function as a risk factor for cardiovascular disease. Curr Atheroscler Rep 2003 5 6 506 13
21. V Schachinger, M. B Britten, A. M Zeiher, Prognostic impact of coronary vasodilator dysfunction on adverse long-term outcome of coronary heart disease. Circulation 2000 101 1899 906
22. D. S Celermajer, K. E Sorensen, Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet 1992 340 1111 15
23. V. G Lelyuk, S. E Lelyuk, The technique of ultrasound examination of the vascular system: scanning technology and regulatory indicators. Textbook: 2002
24. I Campbell, Type 2 diabetes mellitus: «The silent killer». Practical Diabetes Int 2001 18 6 187 91
25. J. A Suwaidi, S Hamasaki, S. T Higano, et al Long-term follow-up of patients with mild coronary artery disease and endothelial dysfunction. Circulation 2000 101 948 54
26. A. A Zateyshchikova, D. A Zateyshchikov, Endothelial regulation of vascular tone: setting, and clinical significance. Cardiology 1998 9 68 80
27. I. P Tatarchenko, N. V Pozdnyakova, A. G Mordovina, O. I Morozova, Dysfunction of vascular endothelium in the evaluation of episodes of myocardial ischemia in type 2 diabetes. Problems of Endocrinology 2009 6 7 11
28. V Dzau, The cardiovascular continuum and rennin-angiotensin-aldosterone system blocade. Hypertens J 2005Suppl): 9 17
29. G Bakris, Comparison of telmisartan vs. valsartan in the treatment of mild to moderate hypertension using ambulatory blood pressure monitoring. J Clin Hypertension 2002Suppl. 1): 26-31.
30. R. A Velliquette, P Ernsberger, Contrasting metabolic effects of antihypertensive agents. J Pharmacol Exp Ther 2003 307 1104 11
31. E. E Dedov, A. A Aleksandrov, Diabetes mellitus and AT1-receptor antagonists: in search of solution. Russian Journal of Medicine 2005 11 11 16
32. J Karalliedde, G Viberti, Evidence for renoprotection by blockade of the renin-angiotensin-aldosterone system in hypertension and diabetes. J Hum Med 2006 35 890 99
33. T Lau, P. O Carlsson, P. S Leung, Evidence for local angiotensin-generating system and dose-dependent inhibition of glucose-stimulated insulin release by angiotensin II in isolated pancreatic islets. Diabetologia 2004 47 240 48
34. O Chung, T Unger, Angiotensin II receptor blockade and end organ protection. Amer J Hypertension 1999 12 150 56
35. I. P Tatarchenko, N. V Pozdnyakova, A. G Mordovina, O. I Morozova, S. A Sekerko, I. A Petrushin, Clinical and functional assessment of organ-protective effectiveness of enalapril and telmisartan among patients with hypertension. Cardiology 2011 4 16 21
36. M Burnier, H Brunner, Angiotensin II receptor antagonists. Lancet 2000 355 637 45
37. D Elmfeld, B Olofsson, P Meredith, The relationships between dose and antihypertensive effect of four AT1-receptor blockers. Differenc in potency and efficacy. Blood Pressure 2002 11 293 301
Kenjaev M.L., Ganiev U. Sh., Abdijalilova S.I., Holov G. Endothelial dysfunction and its correction in patients with ischemic heart disease and diabetes mellitus. International Journal Of Applied And Fundamental Research. – 2013. – № 2 –
URL: www.science-sd.com/455-24268 (24.02.2026).









 PDF
PDF